Health News for the
Well-Read Patient
Wellness
All Articles
Ticked Off: How to Recognize, Relieve and Resist Lyme Disease
Summertime is prime time for ticks, which are becoming more prevalent each year. A combination of changing land use and warmer winters has greatly expanded the ticks’ habitat and they’re…
Ticked Off: How to Recognize, Relieve and Resist Lyme Disease
Summertime is prime time for ticks, which are becoming more prevalent each year. A combination of changing land use and warmer winters has greatly expanded the ticks’ habitat and they’re…
Dementia and Alzheimer’s: Updates from a Leading Geriatrician
Senior Moments Or Something More? As Baby Boomers continue the inexorable journey deep into their senior years, preserving cognitive function understandably tops the list of worries. While Alzheimer’s Disease and…
Dementia and Alzheimer’s: Updates from a Leading Geriatrician
Senior Moments Or Something More? As Baby Boomers continue the inexorable journey deep into their senior years, preserving cognitive function understandably tops the list of worries. While Alzheimer’s Disease and…
Tips for Safe Summer Fun
Stay Safe with Sunscreen, Sunglasses and Plenty of Water The longer, sunshine filled days of summer are upon us and without a doubt, they are one of life’s unrivaled joys,…
Tips for Safe Summer Fun
Stay Safe with Sunscreen, Sunglasses and Plenty of Water The longer, sunshine filled days of summer are upon us and without a doubt, they are one of life’s unrivaled joys,…
Exercise Is Good Medicine
Get Up and Join the Movement As we emerge from the doldrums of winter hibernation and COVID-19-related inertia, it’s important to remember that exercise is good medicine and there’s no…
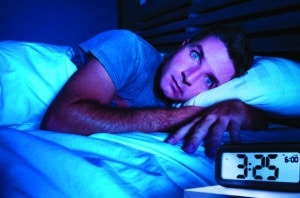
What’s Keeping You Up at Night?
Breaking the Cycle of Anxiety, Insomnia and Sleep Anxiety A good night’s sleep does more than refresh and revitalize. It’s essential to your health, so make it a priority to…
Exercise Is Good Medicine
Get Up and Join the Movement As we emerge from the doldrums of winter hibernation and COVID-19-related inertia, it’s important to remember that exercise is good medicine and there’s no…
What’s Keeping You Up at Night?
Breaking the Cycle of Anxiety, Insomnia and Sleep Anxiety A good night’s sleep does more than refresh and revitalize. It’s essential to your health, so make it a priority to…