Health News for the
Well-Read Patient
All Articles
In a Pickle and Looking for a New Summer Activity?
Try Pickleball, the Country’s Fastest-Growing Sport Tired of the same ‘ole routine every summer but find yourself in a pickle and looking for a new summer activity? Well, according to…
In a Pickle and Looking for a New Summer Activity?
Try Pickleball, the Country’s Fastest-Growing Sport Tired of the same ‘ole routine every summer but find yourself in a pickle and looking for a new summer activity? Well, according to…
Exercise Is Good Medicine
Get Up and Join the Movement As we emerge from the doldrums of winter hibernation and COVID-19-related inertia, it’s important to remember that exercise is good medicine and there’s no…
Exercise Is Good Medicine
Get Up and Join the Movement As we emerge from the doldrums of winter hibernation and COVID-19-related inertia, it’s important to remember that exercise is good medicine and there’s no…
What Does BMI Really Tell Us?
Definitive Diagnostic Tool or Part of a Greater Health Matrix? It’s an easily understood calculation: Body Mass Index, popularly known as BMI, computes an individual’s measure of body fat as…
A Novel Approach to Behavior Change
How to Replace Bad Habits with Healthy, Sustainable Behaviors For entrepreneur physician Kyra Bobinet, MD, the typical reasons behind a failed diet served as the impetus for developing a novel…
Start 2021 off Right by Sticking to your Winter Exercise Plan
A Winter Workout Routine Will Prepare You For Life After COVID Exercise will reduce pain, improve function and mobility, lower blood pressure and blood sugar, decrease risk of chronic illness…
Fighting Fatigue
Wake-up Call: Fighting Fatigue at Its Roots Feel like you are fighting fatigue throughout the day, the joy in life slowly diminishing and your active lifestyle becoming a distant memory?…
Fight Fatigue
Wake-up Call: Fight Fatigue at Its Roots Are these ordinary signs of aging? Exhausted throughout the day, joy in life slowly diminishing, active lifestyle becoming a distant memory. No, no…
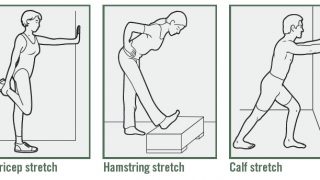
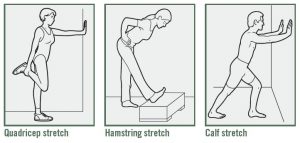
Spring Fitness
Ramping Up your Sprint Fitness after a Long, Sedentary Winter Whether you went into hibernation as the result of a record cold winter season, or took time off from your…