Health News for the
Well-Read Patient
Medications
All Articles
A New Era for Diabetes and Weight Loss Drugs
For patients seeking new solutions to managing type 2 diabetes and obesity, the introduction of a class of drugs called GLP-1 receptor agonists (RA) has simultaneously inspired hope and excitement…
A New Era for Diabetes and Weight Loss Drugs
For patients seeking new solutions to managing type 2 diabetes and obesity, the introduction of a class of drugs called GLP-1 receptor agonists (RA) has simultaneously inspired hope and excitement…
Joint Assets: An Osteoarthritis Update
The aching, swollen, stiff joints associated with osteoarthritis (OA) have long been considered a “wear and tear” condition, associated with aging. It was thought that cartilage, the smooth connective tissue…
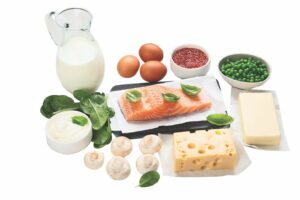
Bone Up: What Is Osteoporosis?
Except for dedicated thespians, saying “break a leg” is most definitely not a harbinger of good luck. More than 10 million Americans are living with osteoporosis, a condition of low…
Joint Assets: An Osteoarthritis Update
The aching, swollen, stiff joints associated with osteoarthritis (OA) have long been considered a “wear and tear” condition, associated with aging. It was thought that cartilage, the smooth connective tissue…
Bone Up: What Is Osteoporosis?
Except for dedicated thespians, saying “break a leg” is most definitely not a harbinger of good luck. More than 10 million Americans are living with osteoporosis, a condition of low…
Pandemic Inspires and Challenges Medical Innovation
Pandemic Sparks Promising Future for Clinical Trial Speed and Flexibility Like wartime medicine, the pandemic inspires and challenges medical innovation. The silver lining of the pandemic is the reinvigorated sense…
COVID-19 Vaccine Update
Experts Weigh In With Reassuring Outlook The COVID-19 vaccine rollout is in full swing around the country but many questions remain. We reveal the latest answers (as of February 2021)…
A Guide to the Power Players in Pain Relief
Which Pain Relievers Work Best? When you reach for a pain reliever, what are you most likely to find in your medicine cabinet? And does it matter? While aspirin, Tylenol…
Antibiotics Awareness is Good for Your Health
Antibiotics Awareness Spurred by Alexander Fleming’s serendipitous discovery of penicillin in 1928, antibiotics have rightfully become wonder drugs, often able to change the course of deadly bacterial infections in a…