Health News for the
Well-Read Patient
Medical Conditions
All Articles
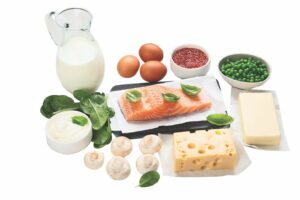
Bone Up: What Is Osteoporosis?
Except for dedicated thespians, saying “break a leg” is most definitely not a harbinger of good luck. More than 10 million Americans are living with osteoporosis, a condition of low…
Bone Up: What Is Osteoporosis?
Except for dedicated thespians, saying “break a leg” is most definitely not a harbinger of good luck. More than 10 million Americans are living with osteoporosis, a condition of low…
What’s Keeping You Up at Night?
Breaking the Cycle of Anxiety, Insomnia and Sleep Anxiety A good night’s sleep does more than refresh and revitalize. It’s essential to your health, so make it a priority to…
What’s Keeping You Up at Night?
Breaking the Cycle of Anxiety, Insomnia and Sleep Anxiety A good night’s sleep does more than refresh and revitalize. It’s essential to your health, so make it a priority to…
Pandemic Stress Likely Compounded by Seasonal Affective Disorder
Coping With Sad This Winter As we continue to weather the storm of COVID-19, seasonal affective disorder, or SAD, is once again on our radar. More subtle than an arctic…
COVID-19 and The Road Ahead
From Boosters & Breakthroughs to Vaccines & Variants: Where Do We Go From Here? The following reflects an 8/24/2021 discussion; please check the CDC website for real-time updates as the…
New Lung Cancer Screening Recommendations
Spotlighting Both Challenges and Progress This winter the U.S. Preventive Services Task Force (USPSTF) released its new Lung Cancer screening recommendations, lowering both the starting age and pack-per-year criteria. Previously,…
A Quick Guide to Seasonal Allergies
Pollen, Grass, Ragweed and Mold spores For more than 24 million Americans, the flowering trees and mild weather of spring and summer, signals another allergy season in full bloom. The…
Can We Co-Exist with COVID-19?
An Epidemiologist Separates Fact from Fiction and Offers Hope for the Future Epidemiologists seek to learn why, how and when some people contract diseases when others don’t. Their findings are used…
Headaches – Types and Remedies
Oh, My Aching Head A dull pressure, a sharp pain, an uncomfortable pounding, a vise-like sensation – all can signal the start of a headache. A painful part of the…